lv unloading | venoarterial ecmo lv unloading lv unloading Data from 686 consecutive patients with cardiogenic shock treated with VA-ECMO with or without left ventricular unloading using an Impella at 16 tertiary care centers in 4 countries were collected. The association between left ventricular unloading and 30-day mortality was assessed by Cox regression models in a 1:1 propensity score–matched .
An electrical system is only as reliable as its conductors and conduit systems & fittings which provide unsurpassed protection for wire and cables in the most demanding applications: power generation, robotics, food processing, refining, waste water treatment, rail rolling stock & trackside, infrastructure, offshore drilling, mining, wind turbin.
0 · venoarterial ecmo unloading criteria
1 · venoarterial ecmo lv unloading
2 · unloading left ventricle ecmo
3 · how to unload left ventricle
Conoce el Sisbén IV. Con la nueva metodología del Sisbén se desarrolló una clasificación cuyo resultado no es un índice cuantitativo. Esto significa que ya no existirá un puntaje de 0 a 100 sino una nueva clasificación que ordena la población por grupos. Se elimina la clasificación por puntaje. El Sisbén IV ordena la población por .
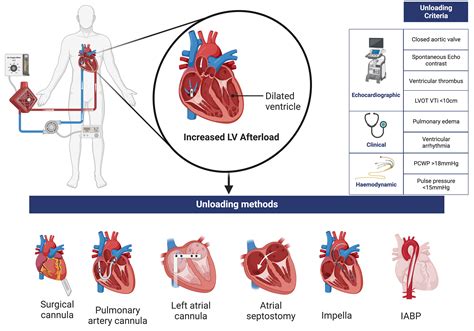
LV unloading refers to strategies that reduce PVA, hence reducing MVO 2 . 10 Unloading has 2 key goals: (1) preventing or treating clinically manifested complications; and (2) promoting LV recovery, even in those . Data from 686 consecutive patients with cardiogenic shock treated with VA . Venoarterial extracorporeal membrane oxygenation (VA-ECMO) use for .The data showed that early LV unloading was associated with significantly lower 30-day .
LV unloading refers to strategies that reduce PVA, hence reducing MVO 2 . 10 Unloading has 2 key goals: (1) preventing or treating clinically manifested complications; and (2) promoting LV recovery, even in those without apparent complications.

Data from 686 consecutive patients with cardiogenic shock treated with VA-ECMO with or without left ventricular unloading using an Impella at 16 tertiary care centers in 4 countries were collected. The association between left ventricular unloading and 30-day mortality was assessed by Cox regression models in a 1:1 propensity score–matched . Venoarterial extracorporeal membrane oxygenation (VA-ECMO) use for circulatory support in cardiogenic shock results in increased left ventricular (LV) afterload. The use of concomitant Impella or intra-aortic balloon pump (IABP) have been proposed as adjunct devices for LV unloading.
The data showed that early LV unloading was associated with significantly lower 30-day mortality (HR, 0.76 (95% CI, 0.60–0.97); p = 0.03), but delayed LV unloading (defined as Impella implantation >2 h after VA ECMO implantation) was not associated with better mortality outcome (HR, 0.77 (95% CI, 0.51–1.16); p = 0.22) . Another light has .ECMO-induced hemodynamics increase cardiac afterload risking left ventricular distention and impaired cardiac recovery. To mitigate potentially harmful effects, multiple strategies to unload the left ventricle (LV) are used in clinical practice but data supporting the optimal approach is presently lacking.LV mechanical unloading (MU) with intra-aortic balloon pump (IABP) or percutaneous ventricular assist device (pVAD) can prevent LV distension, potentially at the risk of more complications, and net clinical benefit remains uncertain.Although cardiopulmonary rescue with peripheral venoarterial extracorporeal membrane oxygenation (VA-ECMO) may be life-saving for patients with acute cardiogenic shock as a bridge to recovery or more durable therapies, adequate left ventricular (LV) unloading is essential to avoid worsening LV distension and its potential sequelae, such as .
venoarterial ecmo unloading criteria
A major shortcoming of VA ECMO is its variable, but inherent increase of left ventricular (LV) mechanical load, which may aggravate pulmonary edema and hamper cardiac recovery. In order to mitigate these negative sequelae of VA ECMO, different adjunct LV unloading interventions have gained a broad interest in recent years. This narrative review elucidates the crucial role of LV unloading in severe cardiogenic shock setting, from the physiological basis to the biomolecular consequences, highlighting the interactions between hemodynamics, . What are the outcomes associated with left ventricular (LV) mechanical unloading (MU) in patients supported with venoarterial extracorporeal membrane oxygenation (VA-ECMO)?
LV unloading refers to strategies that reduce PVA, hence reducing MVO 2 . 10 Unloading has 2 key goals: (1) preventing or treating clinically manifested complications; and (2) promoting LV recovery, even in those without apparent complications. Data from 686 consecutive patients with cardiogenic shock treated with VA-ECMO with or without left ventricular unloading using an Impella at 16 tertiary care centers in 4 countries were collected. The association between left ventricular unloading and 30-day mortality was assessed by Cox regression models in a 1:1 propensity score–matched . Venoarterial extracorporeal membrane oxygenation (VA-ECMO) use for circulatory support in cardiogenic shock results in increased left ventricular (LV) afterload. The use of concomitant Impella or intra-aortic balloon pump (IABP) have been proposed as adjunct devices for LV unloading.The data showed that early LV unloading was associated with significantly lower 30-day mortality (HR, 0.76 (95% CI, 0.60–0.97); p = 0.03), but delayed LV unloading (defined as Impella implantation >2 h after VA ECMO implantation) was not associated with better mortality outcome (HR, 0.77 (95% CI, 0.51–1.16); p = 0.22) . Another light has .
ECMO-induced hemodynamics increase cardiac afterload risking left ventricular distention and impaired cardiac recovery. To mitigate potentially harmful effects, multiple strategies to unload the left ventricle (LV) are used in clinical practice but data supporting the optimal approach is presently lacking.
LV mechanical unloading (MU) with intra-aortic balloon pump (IABP) or percutaneous ventricular assist device (pVAD) can prevent LV distension, potentially at the risk of more complications, and net clinical benefit remains uncertain.
Although cardiopulmonary rescue with peripheral venoarterial extracorporeal membrane oxygenation (VA-ECMO) may be life-saving for patients with acute cardiogenic shock as a bridge to recovery or more durable therapies, adequate left ventricular (LV) unloading is essential to avoid worsening LV distension and its potential sequelae, such as . A major shortcoming of VA ECMO is its variable, but inherent increase of left ventricular (LV) mechanical load, which may aggravate pulmonary edema and hamper cardiac recovery. In order to mitigate these negative sequelae of VA ECMO, different adjunct LV unloading interventions have gained a broad interest in recent years.
replica watch brands uk
This narrative review elucidates the crucial role of LV unloading in severe cardiogenic shock setting, from the physiological basis to the biomolecular consequences, highlighting the interactions between hemodynamics, .
replica watch store los angeles
venoarterial ecmo lv unloading
unloading left ventricle ecmo
Download this manual. LINEA. ™. by HALO. LV 8 0 9 P. LV 8 0 3 P. 272. COOPER LIGHTING. ®. LV 8 0 9 P. 3 Light - White Ellipse kit. Includes three lampholders with 35W. MR11 lamps, two 3' sections of track. (32 3/16" actual length), one canopy. mount power supply, lamps and all. necessary hardware in an attractive full. color display package.
lv unloading|venoarterial ecmo lv unloading